Young and Late-onset Parkinson’s Disease (YLOPD) Study

SKAN Research Trust, a public charitable trust set up by the Soota and Karedan families, aims to promote research and development in medical science, with a focus on the treatment of geriatric and neurological diseases. As SKAN’s strategic partner for neurological research, CBR has built a consortium of scientists and clinicians to plan and carry out a project on Parkinson’s disease, which is the first among several clinical areas of research that will be pursued through this exciting collaboration.
The ‘Young and Late-onset Parkinson’s Disease’ (YLOPD) study is a longitudinal study on Parkinson’s disease (PD), the second most common neurodegenerative disorder characterized by slowness in movements and impaired posture and balance. PD has a prolonged course with slow and gradual progression. It is caused by the degeneration of nerve cells in a part of the brain called substantia nigra, and the loss of the ability to produce a key neurotransmitter called dopamine. PD typically manifests around the age of 60 and is more prevalent in men than women, with a 50% higher risk.
Funded by the SKAN Research Trust, the study began in 2021 as a collaborative undertaking between CBR and the National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru. This study aims to recruit 1000 patients with young and late-onset PD and follow them up periodically to study the natural history of the disease.
Existing literature shows that people who develop young-onset PD (YOPD) have different initial symptoms, non-motor symptoms, environmental risk factors, rate of progression, choice of deep brain stimulation target, and quality of life impairment as compared to late-onset PD (LOPD). Growing evidence highlights the importance of YOPD and LOPD and their impact on a person’s quality of life. However, the multifactorial causation, neuroanatomical features, and genetic architecture of YOPD and LOPD are not fully understood; the YLOPD study strives to address this crucial gap.
The YLOPD study involves comprehensive multimodal evaluation of clinical, electrophysiological, and cognitive functions, brain and retinal imaging, genome-wide association and whole genome sequencing, blood-based inflammatory and protein biomarkers, and studies on heavy metal and pesticide exposure with emphasis on differential involvement in YOPD and LOPD.
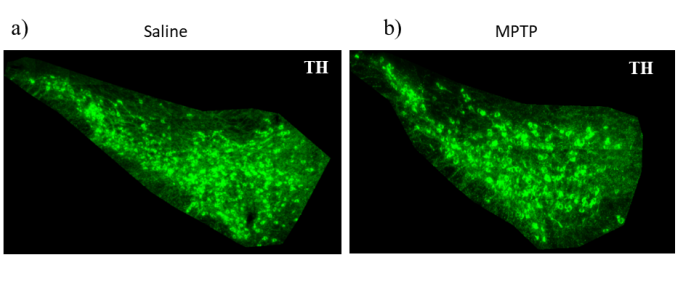
The study is focused on linking the insights from clinical literature to explore translational research in animal models of PD in order to decipher molecular underpinnings of the emergence of non-motor symptoms (NMS) and motor symptoms (MS). In PD it is known that degeneration of substantia nigra (SNpc) dopaminergic neurons and their projections to striatum causing dopamine depletion is associated with MS. However, a broad spectrum of neuropsychiatric symptoms, including NMS (like anxiety and depression) frequently observed in PD, are probably related to other non-dopaminergic neurons and their projections to target regions in the brain. The etiology, in terms of aggregation of the presynaptic protein alpha-synuclein in Lewy bodies or in the neurites that may contribute to NMS, is not clear. We are using the MPTP (1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine hydrochloride) neurotoxicity mouse model of PD at sub-chronic dosing and alpha-synuclein- dependent progressive disease mice model of PD to understand the molecular basis for the emergence of these NMS.
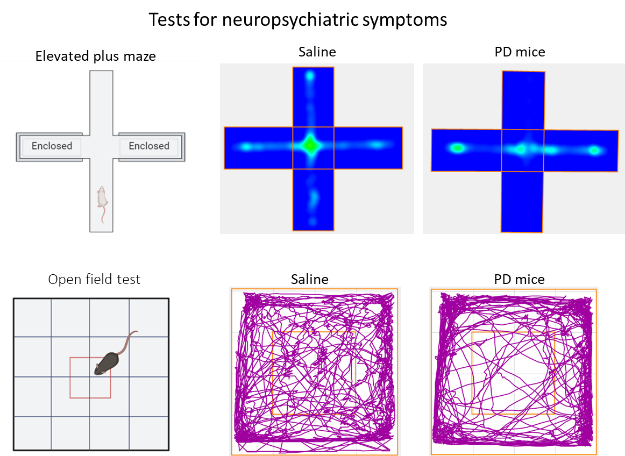

To investigate non-motor symptoms, mice are subjected to a series of behavioural tests such as the elevated plus maze, open field test, and forced swim test. These tests allow us to assess anxiety- and depression-like behaviours. Tests such as the rotarod test, tail swing test, and beam walk test aid in the assessment of motor coordination and balance in the mice. Data from these experiments, together with those from histopathology analyses and complementary studies, would lead to a comprehensive view of the potential mechanisms of disease progression.
We hope that this ‘bench-to-bedside’ study will shed light on many unanswered questions on PD which can be effectively used to support the implementation of effective interventions and modification of existing treatment protocols.
Last Updated on August 8, 2023